Colorectal Cancer: Diagnosis and Treatment
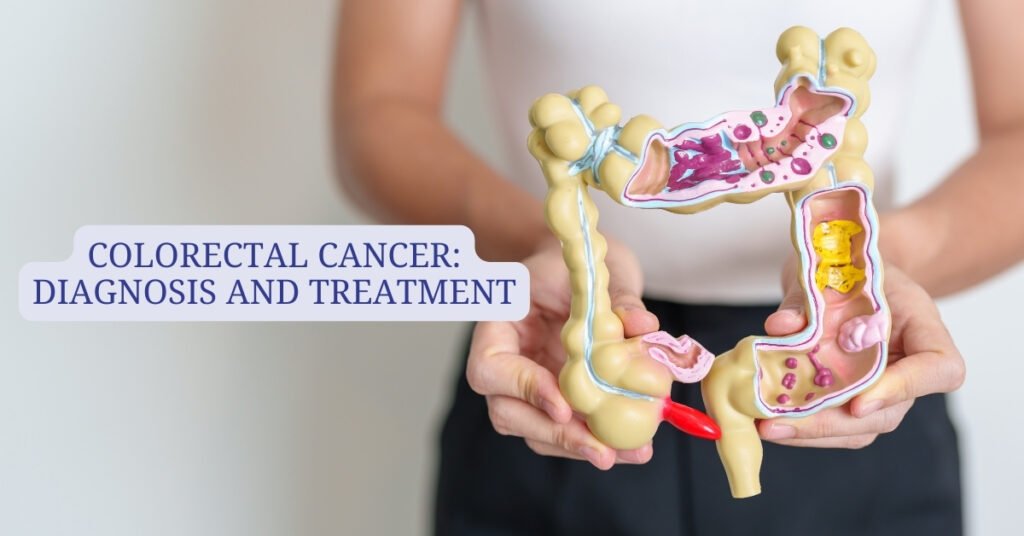
Colorectal cancer is a severe health concern that affects millions of people around the world. It can manifest in a variety of ways, including changes in bowel habits, blood from the rectum, abdominal pain, or loss of weight without reason. Identifying it early and seeking prompt treatment is incredibly important for preventing it from becoming worse and impacting your life. Let’s explore how colorectal cancer is diagnosed and treated.
How is colorectal cancer diagnosed?
Early detection of colorectal cancer is critical for successful treatment. Screening should help to identify polyps prior to their turning into cancer and detect colorectal cancer at an early stage when treatment is most effective. About 80% of colorectal cancer is diagnosed after symptoms that trigger a colonoscopy, in about 11% of cases, routine screening identifies the cancer; and in about 7% of the cases, the person is diagnosed through emergency care for sudden abdominal symptoms.
Recent posts
Recognizing the Symptoms of Multiple Myeloma Early Multiple myeloma, a type of blood cancer, is a rare but serious condition that affects …
Home >> Colorectal Cancer Awareness Month: Educate, Prevent, and Detect Early What is Colorectal Cancer Awareness Month? Colorectal Cancer Awareness Month is …
Common Screening and Diagnostic Procedures
- Colonoscopy: The most sensitive diagnostic test is the colonoscopy. With the use of a colonoscope containing a camera and light, the doctors can better see, take a tissue sample, or remove polyps for further testing.
- Blood Stool Test: This test looks for signs of blood in the stool, and while these results may be indicative of other conditions, it is used to detect cancer.
- Stool immunochemistry: This is a test that finds hidden blood in the lower portion of the colon. This test is used to detect early signs of cancer.
- Stool DNA Test: In this test, the doctors look for DNA markers shed by colorectal cancer or precancerous polyps in the stool. This test provides the answers to the potential malignancy, and if it is positive, further evaluation will be necessary.
- Flexible sigmoidoscopy: This is a minimally invasive procedure that uses a flexible tube to visualize the rectum and sigmoid colon. This procedure helps the doctors get excellent diagnostic information.
- Barium Enema X-ray: In this procedure, barium dye is used to highlight any abnormal features on X-rays of the colon. This procedure helps the doctors diagnose the conditions.
- CT colonography: This procedure produces detailed images of the colon. Because it is less invasive than colonoscopy, this procedure requires further evaluation if abnormalities are detected.
- Imaging scans: Ultrasound, CT, or MRI scans are used to evaluate the extent of cancer spread beyond the colon.
What are the management and treatment options for colorectal cancer?
The management of colorectal cancer depends on many factors: the size, location, stage of malignancy, the individual’s recurrence, and his general health. Management options include chemotherapy, radiation therapy, surgical intervention, and palliative care to alleviate symptoms and promote quality of life.
- Surgical Management:
Surgical treatment is the mainstay of management for local colorectal malignancy, and the main goal is the excision of malignant tissue, including tumors and regional lymph nodes, to prevent metastatic disease. Sometimes, surgeons reconnect the bowel after excision of the tumors and sometimes create a diversion stoma to divert the feces into a colostomy bag. The techniques of surgery may vary from open procedures with large incisions to laparoscopic or mini-incision approaches, where the surgeon has the help of robotic assistance. Standard surgical procedures include local excision, colectomy (partial and total), and symptomatic obstructions.
- Chemotherapy:
The use of drugs to kill cancer cells throughout the body is known as chemotherapy. It may be used as a single treatment or to shrink the tumor before resection. Chemotherapy causes overall side effects due to its effect on normal cells in addition to cancerous cells.
- Targeted Therapy:
Targeted therapy uses drugs targeted at proteins that regulate the growth of cancer cells. It offers a more selective approach with reduced side effects compared with chemotherapy.
- Immunotherapy:
Immunotherapy uses drugs to stimulate the immune system’s ability to recognize and kill cancer cells. This treatment modality shows promising applicability for advanced colorectal malignancy; however, it may be associated with autoimmune reactions.
- Radiation Therapy:
Radiation therapy targets high-energy beams to destroy cancer cells and delay their proliferation. It is commonly used before rectal cancer resection or to improve treatment results as part of a combination with chemotherapy.
- Ablation techniques:
Ablation techniques include microwaves, radiofrequency, ethanol, or cryosurgery to destroy the tumors without surgically removing them, providing a minimally invasive alternative in cases of particular presentation.
- Palliative care:
In cases where the colorectal cancer has reached an advanced stage and curative treatment is not viable, palliative care targets the reduction of symptoms, including pain, nausea, and diarrhea, and support for emotional well-being. The treatment will include surgical interventions and radiation therapy to reduce the tumor, chemotherapy for the same, and supportive measures, including counseling and care in a hospice.
Preventing Colorectal Cancer
- Lifestyle Changes and Screening:
Proactive lifestyle changes and screening significantly reduce the risk of colorectal cancer. The lifestyle changes involve a diet high in fruits and vegetables, avoiding the use of tobacco, leading an active lifestyle, limiting alcohol intake, and avoiding exposure to environmental hazards. Suspected colorectal cancer symptoms should be promptly evaluated and diagnosed by one’s healthcare provider.
- Importance of regular screening:
Regular screening plays a critical role in detecting colorectal cancer at an early stage, when treatment is most effective. Studies have shown that screening reduces the incidence and mortality rates of colorectal cancer by detecting and removing precancerous growths. Stool-based testing, such as the fecal occult blood test (FOBT), provides an easily administered, non-invasive method of detecting hidden blood in the stool, which may signify the presence of colorectal cancer or polyps. Further diagnostic procedures, like colonoscopy, are advised if abnormalities are found during stool-based testing.
- Genetic counseling and testing:
Individuals who have a family history of colorectal cancer or specific genetic conditions should consider the effects of genetic counseling and testing in understanding their risks and the appropriate patterns of screening. Knowledge of one’s predispositions to colorectal cancer has immense implications for personal precautions and the time for early detection and intervention.
- Preventive risk factors:
Though colorectal cancer cannot be prevented entirely, risk factors can be managed to minimize the probability of colorectal cancer. For example, preventing tobacco use and moderating alcohol consumption, weight management, eating a balanced diet rich in fruits, vegetables, and whole grains, and maintaining a certain level of physical activity should be undertaken. In addition, knowledge of family medical history combined with adherence to the colorectal cancer screening guidelines will help in early detection and intervention for such people who are at risk through a family predisposition for colorectal cancer.
- Consulting an expert:
Healthcare provider consultation is of crucial importance to navigate the challenges of colorectal cancer diagnosis, treatment, and prognosis. Being able to ask questions that are relevant to cancer type, stage, treatment options, and any side effects associated with treatment, as well as the likelihood of recurrence, provides an opportunity to make informed decisions about treatment and care. In addition, discussing the possibilities of clinical trials or newer treatment options may also provide opportunities for personalized treatment.
- Self-care and follow-up:
Self-care is critical for colorectal cancer survivors, tailored to their needs. Patients treated for early-stage cancer often transition to being cured but often worry about recurrence. Patients with advanced cancer, on the other hand, often focus on managing symptoms through treatments such as palliative care. Routine follow-up care, including colonoscopies and tests, is critical for the early detection of recurrence or progression of the disease.
In summary, coping with colorectal cancer demands intensive collaboration between patients and healthcare providers, including discovery, active surveillance, and treatment selection. By emphasizing education, frequent follow-up, and a greater understanding of the disease, we can learn to help patients with colorectal cancer maintain good health.
About Author
Dr. A. Venugopal
MD (General Medicine), DM (Medical Oncology), MRCP – SCE Medical Oncology (UK), ECMO (Switzerland).
Dr A. Venugopal is One of the best medical oncologist and Hemato Oncologist in hyderabad, currently serving as the Head of the Department and Senior Medical Oncologist, Hemato Oncologist at Pi Health Cancer Hospital in Gachibowli, Hyderabad. He brings over 15 years of extensive experience in the field of Oncology.